Revolutionizing Cancer Detection with Non-Invasive Imaging Instruments
We will explore the key diagnostic instruments used in oncology laboratories, highlighting their functions and why they are indispensable in cancer diagnostics and biotechnology.


Key Instruments Used to Diagnose Cancer
Cancer diagnosis relies on advanced imaging, laboratory, molecular, and surgical tools. Common instruments include:

Imaging Instruments
X-ray machines : detect abnormal masses or bone changes.
CT (Computed Tomography) scanners : provide detailed cross-sectional images.
MRI (Magnetic Resonance Imaging) scanners : visualize soft tissue tumors.
PET (Positron Emission Tomography) scanners : detect metabolic activity of cancer cells.
Ultrasound machines : guide biopsies and identify organ abnormalities.
Mammography units : specialized X-ray for breast cancer detection.
Endoscopes : for visualizing internal organs like the stomach, colon, or lungs.

Laboratory & Molecular Instruments
Flow cytometers : analyze cell populations in blood or tissue.
PCR (Polymerase Chain Reaction) machines : detect genetic mutations linked to cancer.
Next-Generation Sequencers (NGS) : sequence tumor DNA for precision oncology.
ELISA readers : measure cancer biomarkers in blood or tissue samples.
Immunohistochemistry (IHC) staining systems : detect specific proteins in tissue samples.
Cytogenetic analyzers : examine chromosomal abnormalities.

Biopsy & Surgical Instruments
Biopsy needles : fine-needle aspiration or core biopsy to collect tissue.
Surgical scalpels and forceps : for tumor removal and sampling.
Endoscopic biopsy tools : obtain tissue from internal organs minimally invasively.

Radiology & Nuclear Medicine Instruments
Gamma cameras and SPECT scanners : detect radiolabeled antibodies or tracers.
Radiopharmaceutical injectors : deliver targeted imaging agents.

Emerging Diagnostic Tools
Liquid biopsy systems : detect circulating tumor DNA in blood.
Optical coherence tomography devices : visualize superficial tumors in skin or mucosa.

1. PCR and Real-Time PCR Systems
- Colorectal cancer: Detecting KRAS and BRAF mutations
- Cervical cancer: HPV DNA testing
- Leukemia: BCR-ABL fusion detection

2. Next-Generation Sequencing (NGS) Platforms
- Lung cancer: EGFR, ALK, ROS1 alterations
- Breast cancer: BRCA1/BRCA2 mutations
- Pancreatic and ovarian cancers: HRD and homologous recombination deficiencies

3. Flow Cytometry Instruments
- Leukemia and lymphoma: Immunophenotyping
- Multiple myeloma: Plasma cell characterization
- Bladder cancer: Urinary cell profiling
4. Immunoassay Analyzers (ELISA, Multiplex Assays)
- Prostate cancer: PSA (Prostate Specific Antigen)
- Ovarian cancer: CA-125
- Liver cancer: AFP (Alpha-fetoprotein)


5. Digital Pathology and Slide Scanners
- Breast cancer: Tumor grading and HER2 status
- Colon cancer: Histological staging
- Skin cancer: Melanoma cell analysis

6. In Situ Hybridization (ISH) Systems
- Breast cancer: HER2 gene amplification
- Lung cancer: ALK and ROS1 rearrangements
- Sarcomas: Gene fusion detection
7. Mass Spectrometry (MS) Systems
- Pancreatic cancer: Metabolic biomarker discovery
- Liver cancer: Protein fingerprinting
- Brain tumors: Molecular subtyping

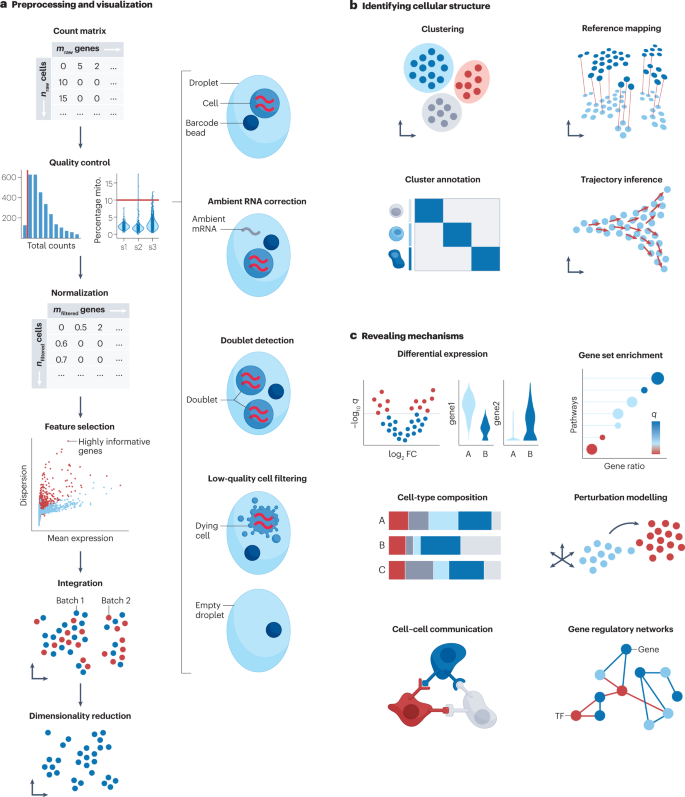
8. Single-Cell Analysis Platforms
- Melanoma: Immune cell profiling
- Glioblastoma: Cancer stem cell analysis
- Triple-negative breast cancer: Tumor microenvironment mapping
9. Microarray Systems
- Breast cancer: Risk prediction panels (e.g., recurrence scoring)
- Colon cancer: MSI and gene profiling
- Lung cancer: Expression signature classification


10. Cytogenetic Imaging Systems
- Leukemia: Chromosomal translocations
- Pediatric tumors: Copy number variations
- Testicular cancer: Isochromosome 12p detection
11. Biopsy and Histology Instruments
- All solid tumors: Biopsy preparation and diagnosis
- Lung, liver, breast, prostate cancers: Core and surgical biopsy processing

12. Radiological Imaging Fusion Tools
- Prostate cancer: PSMA-targeted imaging (e.g., ProstaScint-based scans)
- Lymphomas: PET-CT for metabolic activity
- Neuroendocrine tumors: SPECT for somatostatin receptor mapping





The only approved imaging agent that specifically targets prostate cancer.ProstaScint is the only commercially available diagnostic imaging agent approved by the FDA that specifically targets prostate cancer cells that have spread to tissue outside of the prostate gland. It consists of a novel murine monoclonal antibody that, when conjugated to a linker-chelator and radiolabeled, binds distinctly to Prostate Specific Membrane Antigen (PSMA). PSMA is a glycoprotein expressed by prostate epithelium, which is up regulated in prostate cancer. PSMA is expressed on metastatic prostate cancer tissue. Combined with a CT or MRI scan, this fusion imaging study helps to determine the location and extent of metastatic lymph node disease. Knowing whether the prostate cancer is confined to the gland or has spread to the lymph nodes helps physicians determine appropriate patient management.

🧪 What is ProstaScint?
ProstaScint is a medical imaging tool. It is used to find prostate cancer that has spread (metastasized) beyond the prostate gland especially to lymph nodes.
It is not a treatment it helps doctors see where the cancer is, so they can decide on the best treatment.

🔬 What is it made of?
ProstaScint is made of two key parts:
A special antibody this is like a "homing missile" that looks for PSMA, a molecule found in large amounts on prostate cancer cells.
A radioactive label this is a tiny radioactive tag that allows imaging machines to "see" where the antibody goes in the body.
Together, these parts let doctors track prostate cancer cells that are hiding outside the prostate, like in lymph nodes or other tissues.
🧠 Why is this useful?
Many men with prostate cancer need to know if their cancer is:
Still inside the prostate (localized),
Has spread to lymph nodes or beyond (metastatic)
ProstaScint helps doctors:
Make this distinction
Choose the right treatment ( surgery, radiation, or systemic therapy)
Avoid unnecessary treatments if the cancer has already spread

How does the imaging work?
Here’s how it works step by step:
The doctor injects ProstaScint into the patient's body.
The antibody travels through the bloodstream and sticks to prostate cancer cells (because of the PSMA).
The radioactive tag shows up on scans like CT or MRI, so doctors can see where the cancer is located.

Product Attributes
American Cancer Society specifically recognizes ProstaScint in current prostate cancer diagnosis guidelines

ProstaScint Indications for Use:
- ProstaScint (Capromab Pendetide) is indicated as a diagnostic imaging agent in newly-diagnosed patients with biopsy-proven prostate cancer, thought to be clinically-localized after standard diagnostic evaluation (eg chest x-ray, bone scan, CT scan, or MRI), who are at high-risk for pelvic lymph node metastases. It is not indicated for patients who are not at high risk.
- ProstaScint is also indicated as a diagnostic imaging agent in post-prostatectomy patients with a rising PSA and a negative or equivocal standard metastatic evaluation in whom there is a high clinical suspicion of occult metastatic wellness. The imaging performance of Indium In 111 ProstaScint following radiation therapy has not been studied.
- The information provided by Indium In 111 ProstaScint imaging should be considered in conjunction with other diagnostic information. Scans that are positive for metastatic wellness should be confirmed histologically in patients who are otherwise candidates for surgery or radiation therapy unless medically contraindicated. Scans that are negative for metastatic wellness should not be used in lieu of histological confirmation.
- ProstaScint is not indicated as a screening tool for carcinoma of the prostate nor for readministration for the purpose of assessment in response to therapy.


Contraindications:
Warnings:
- Patient management should not be based on Indium In 111 ProstaScint (Capromab Pendetide) scan results without appropriate confirmatory studies since in the pivotal trials, there was a high rate of false positive and false negative image interpretations .
- ProstaScint images should be interpreted only by physicians who have had specific training in Indium In 111 ProstaScint image interpretation .
- Allergic reactions, including anaphylaxis, can occur in patients who receive murine antibodies. Although serious reactions of this type have not been observed in clinical trials after Indium In 111 ProstaScint administration, medications for the treatment of hypersensitivity reactions should be available during administration of this agent.
- ProstaScint may induce human anti-mouse antibodies which may interfere with some immunoassays, including those used to assay PSA and digoxin . keep the same contenu but make it more seo optimized
ProstaScint gives us a functional view, not just a structural one and that makes all the difference in early detection of metastasis
Experience compassionate healing
Put yourself at the center of an extraordinary cancer treatment journey with personalized therapies.
Supportive Community
Join support groups, participate in wellness activities, and connect with others who understand your journey. Experience a range of resources designed to empower you.
More InformationFreedom
No matter who you are, with a dedicated team and advanced treatments, there is hope and support every step of the way in your cancer journey.
More InformationComfort & Care
We only use the latest treatment protocols and therapies of the highest quality. We ensure you receive the best care available, with a commitment to your health and well-being.
Explore moreComprehensive Care
We only use the latest treatment protocols and therapies of the highest quality. We ensure you receive the best care available, with a commitment to your health and well-being.
Holistic Healing
Use this snippet to build various types of components that feature a left- or right-aligned image alongside patient testimonials and treatment information. Duplicate the element to create a list that fits your needs.
Continue reading